Claudication, characterized by pain or discomfort in the legs during physical activity, is a symptom that can stem from two distinct causes: neurological claudication and vascular claudication. As a board-certified neurosurgeon with over 20 years of experience, I frequently encounter patients confused about whether their leg pain is due to a nerve issue or a vascular problem. Accurate diagnosis is critical, as treatments differ significantly. Neurological claudication, often caused by spinal conditions like lumbar spinal stenosis, affects 1–6% of adults over 60, while vascular claudication, linked to peripheral artery disease (PAD), impacts 10–20% of the same age group (American Academy of Neurology, 2024; American Heart Association, 2024).
This detailed guide, updated for 2025, compares neurological and vascular claudication, covering causes, symptoms, diagnosis, treatment, and management strategies. Designed with clear explanations, case studies, and visuals, it aims to empower patients to seek appropriate care. For expert evaluation in Madurai, consult Dr. Shyam D at drshyam.com. Always seek professional medical advice for leg pain or related symptoms.
Disclaimer: This article is for informational purposes only and not a substitute for medical advice. Consult a healthcare professional for diagnosis and treatment.
Introduction
Claudication, derived from the Latin word for “limping,” manifests as leg pain, cramping, or weakness triggered by walking or exercise, typically relieved by rest. While both neurological and vascular claudication share this hallmark, their origins differ:
- Neurological Claudication (also called neurogenic claudication): Caused by nerve compression, often from lumbar spinal stenosis, impeding nerve signals to the legs.
- Vascular Claudication: Result of reduced blood flow due to peripheral artery disease (PAD), starving leg muscles of oxygen during activity.
Misdiagnosis can delay effective treatment, worsening symptoms or complications. This guide clarifies the differences, helping patients identify the right specialist—neurologists/neurosurgeons for neurological issues or vascular surgeons for PAD. With insights from clinical data and patient stories, we’ll explore how to navigate these conditions, featuring expertise from Dr. Shyam D in Madurai.
Visual Suggestion: Include an infographic comparing neurological vs. vascular claudication (causes, symptoms, treatments).
What Is Neurological Claudication?
Neurological claudication, or neurogenic claudication, arises from compression of spinal nerves, typically in the lumbar spine (lower back). It’s most commonly associated with lumbar spinal stenosis, where the spinal canal narrows, pressing on nerves.
Causes
- Lumbar Spinal Stenosis: Age-related degeneration of spinal discs, ligaments, or joints (affects 1–6% of adults over 60).
- Herniated Discs: Discs bulging into the spinal canal, compressing nerves.
- Spondylolisthesis: Vertebrae slipping out of alignment, narrowing nerve space.
- Tumors or Cysts: Rare, but spinal growths can compress nerves.
- Trauma: Injuries causing spinal misalignment or swelling.
Symptoms
- Pain Type: Cramping, aching, or burning in the legs, buttocks, or lower back.
- Triggers: Walking, standing, or extending the spine (e.g., leaning back).
- Relief: Sitting, leaning forward, or resting (the “shopping cart sign”—relief when bending forward).
- Associated Signs: Numbness, tingling, or weakness in the legs; symptoms are often bilateral.
- Location: Pain radiates from the lower back to the thighs or calves.
Key Characteristics
- Symptoms worsen with spinal extension and improve with flexion.
- No significant skin or temperature changes in the legs.
- Normal pulses in the feet, as blood flow is unaffected.
Case Study: A 65-year-old patient with lumbar spinal stenosis experienced leg pain after walking 100 meters, relieved by sitting. Dr. Shyam D in Madurai performed a laminectomy, resolving symptoms within 6 weeks (drshyam.com, 2024).
What Is Vascular Claudication?
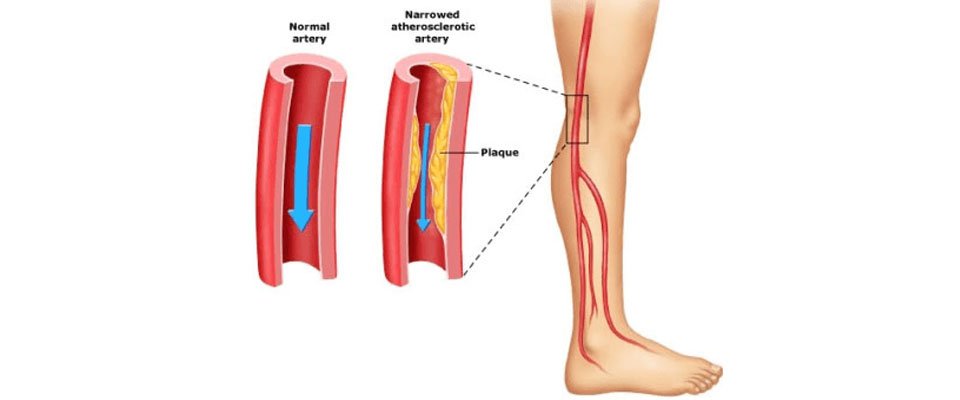
Vascular claudication results from reduced blood flow to the leg muscles, primarily due to peripheral artery disease (PAD), where arteries narrow from atherosclerosis (plaque buildup).
Causes
- Peripheral Artery Disease: Affects 10–20% of adults over 60; risk factors include smoking, diabetes, hypertension, and high cholesterol (American Heart Association, 2024).
- Arterial Thrombosis: Blood clots blocking leg arteries.
- Aneurysms: Rare, but weakened artery walls can reduce blood flow.
- Vasculitis: Inflammation of blood vessels, restricting flow.
Symptoms
- Pain Type: Tightness, cramping, or aching in the calves, thighs, or buttocks (muscle-specific).
- Triggers: Walking or exercise, with pain appearing after a consistent distance (e.g., 200 meters).
- Relief: Stopping activity for 1–5 minutes, without needing to sit or change posture.
- Associated Signs: Cool skin, hair loss on legs, weak pulses, or leg discoloration (pale or bluish).
- Location: Pain is localized to muscle groups (e.g., calves), often unilateral.
Key Characteristics
- Symptoms are exertion-dependent, not posture-related.
- Physical signs like weak pulses or skin changes indicate vascular issues.
- Pain distance is predictable (e.g., “claudication distance”).
Case Study: A 70-year-old smoker with PAD experienced calf pain after walking 150 meters. A vascular surgeon performed an angioplasty, restoring blood flow and eliminating pain within 4 weeks (Cleveland Clinic, 2024).
Visual Suggestion: Include a table comparing neurological vs. vascular claudication symptoms.
Table: Neurological vs. Vascular Claudication
| Feature | Neurological Claudication | Vascular Claudication |
|---|---|---|
| Cause | Nerve compression (e.g., spinal stenosis) | Reduced blood flow (e.g., PAD) |
| Pain Type | Cramping, burning, aching | Tightness, cramping in muscles |
| Triggers | Walking, standing, spinal extension | Walking, exercise |
| Relief | Sitting, leaning forward | Stopping activity (1–5 min) |
| Associated Signs | Numbness, tingling, weakness | Cool skin, weak pulses, hair loss |
| Location | Back to legs, often bilateral | Calves, thighs, unilateral or bilateral |
| Physical Exam | Normal pulses, no skin changes | Weak pulses, cool or pale skin |
Diagnosis: Differentiating Neurological and Vascular Claudication
Accurate diagnosis is essential, as treatments differ significantly. Specialists use a combination of clinical evaluation and diagnostic tests:
Neurological Claudication Diagnosis
- Clinical Exam: Assess posture-related pain, reflexes, and sensory changes.
- Imaging:
- MRI/CT: Identifies spinal stenosis, herniated discs, or tumors.
- X-rays: Detects spinal misalignment or degeneration.
- Electrodiagnostic Tests: Nerve conduction studies or EMG to evaluate nerve function.
- Specialist: Neurologists or neurosurgeons like Dr. Shyam D (drshyam.com).
Vascular Claudication Diagnosis
- Clinical Exam: Check pulses, skin temperature, and leg appearance.
- Ankle-Brachial Index (ABI): Measures blood pressure ratio in legs vs. arms (normal: 0.9–1.3; PAD: <0.9).
- Imaging:
- Doppler Ultrasound: Assesses blood flow in arteries.
- Angiography: Visualizes arterial blockages.
- Blood Tests: Evaluate cholesterol, diabetes, or inflammation markers.
- Specialist: Vascular surgeons or cardiologists.
Key Differentiator: Neurological claudication involves posture-dependent pain with normal pulses, while vascular claudication is exertion-dependent with vascular signs (weak pulses, cool skin).
Case Study: A 62-year-old patient with leg pain was misdiagnosed with vascular claudication. Dr. Shyam D’s MRI revealed spinal stenosis, and a decompression surgery resolved symptoms, highlighting the need for accurate diagnostics (drshyam.com, 2024).
Visual Suggestion: Include a flowchart for diagnosing claudication (e.g., symptoms → physical exam → imaging).
Treatment Options
Neurological Claudication Treatments
- Conservative:
- Physical Therapy: Core strengthening and posture exercises (e.g., flexion-based stretches) improve symptoms in 50–60% of cases (PMC, 2024).
- Medications: NSAIDs, gabapentin, or epidural steroid injections for pain relief.
- Lifestyle: Weight loss and avoiding spinal extension activities.
- Surgical:
- Laminectomy: Removes bone/ligament to decompress nerves (70–85% success rate).
- Spinal Fusion: Stabilizes spine in severe cases.
- Minimally Invasive: Endoscopic decompression, offered by experts like Dr. Shyam D, reduces recovery time.
- Recovery: 4–12 weeks for surgical cases; physical therapy may take 6–12 months.
Vascular Claudication Treatments
- Conservative:
- Exercise Therapy: Supervised walking programs increase pain-free walking distance by 50–200% (American Heart Association, 2024).
- Medications: Cilostazol improves blood flow; statins manage cholesterol.
- Lifestyle: Quit smoking, control diabetes, and adopt a heart-healthy diet.
- Surgical/Interventional:
- Angioplasty/Stenting: Opens narrowed arteries (80–90% success rate).
- Bypass Surgery: For severe PAD, rerouting blood flow.
- Recovery: 2–6 weeks for angioplasty; 6–12 weeks for bypass.
Visual Suggestion: Include a side-by-side comparison graphic of treatment options.
Table: Treatment Comparison
| Treatment | Neurological Claudication | Vascular Claudication |
|---|---|---|
| Conservative | Physical therapy, NSAIDs, injections | Exercise therapy, cilostazol, statins |
| Surgical | Laminectomy, spinal fusion | Angioplasty, bypass surgery |
| Success Rate | 70–85% (surgery) | 80–90% (angioplasty) |
| Recovery Time | 4–12 weeks (surgery) | 2–12 weeks |
Managing Claudication: Practical Tips
For Neurological Claudication
- Exercises: Flexion-based stretches (e.g., child’s pose) for 10–15 minutes daily.
- Posture: Use a lumbar roll when sitting; avoid standing for long periods.
- Pain Management: Apply heat to the lower back; consider acupuncture (20–30% pain reduction, PMC, 2024).
- Specialist: Consult neurosurgeons like Dr. Shyam D for surgical or non-surgical plans (+91 63802 71088).
For Vascular Claudication
- Walking Program: Walk to the point of pain, rest, and repeat for 30–60 minutes daily.
- Diet: Increase omega-3s (fish, nuts) and reduce saturated fats.
- Smoking Cessation: Quitting doubles pain-free walking distance (Cleveland Clinic, 2024).
- Specialist: See a vascular surgeon for ABI testing or interventions.
Patient Tip: Keep a symptom diary noting pain triggers, duration, and relief methods to share with your doctor.
When to Seek Medical Help
Seek immediate care if you experience:
- Neurological Claudication:
- Leg weakness, numbness, or loss of bladder/bowel control (cauda equina syndrome).
- Pain worsening despite rest or therapy.
- Vascular Claudication:
- Leg pain at rest, ulcers, or skin discoloration (critical limb ischemia).
- Sudden severe pain (possible arterial clot).
Recommendation: In Madurai, Dr. Shyam D (drshyam.com) offers expert neurological evaluations for claudication, using advanced MRI and minimally invasive techniques.
Neurological claudication stems from nerve compression (e.g., spinal stenosis) and is posture-dependent, while vascular claudication results from poor blood flow (e.g., PAD) and is exertion-dependent.
Neurological pain is relieved by sitting or leaning forward and has normal pulses. Vascular pain is relieved by stopping activity and shows weak pulses or skin changes. Consult a specialist for diagnosis.
Neurological: MRI/CT, nerve conduction studies. Vascular: ABI, Doppler ultrasound, angiography.
Yes, physical therapy and weight loss help neurological claudication; exercise and smoking cessation improve vascular claudication.
Conclusion & Call to Action
Neurological and vascular claudication, while sharing symptoms like leg pain, require distinct diagnoses and treatments. Neurological claudication, often from spinal stenosis, benefits from physical therapy or surgery like laminectomy, while vascular claudication, tied to PAD, responds to exercise and vascular interventions. Accurate diagnosis by specialists like Dr. Shyam D in Madurai ensures effective care. Understanding these differences empowers patients to seek timely treatment and improve quality of life.
